Alterations in the levels of thyroid hormones affect numerous body functions, especially that of the endocrine system.
As a result, thyroid disorders affect the release of hormones, including testosterone.
Testosterone: An Overview
Testosterone is a hormone synthesized in the testes and the adrenal glands. The amount secreted is then regulated by the pituitary gland.
Testosterone is an androgen or male sex hormone that leads to the development of male sex characteristics; the alterations usually seen during the puberty stage in boys.
Through the influence of testosterone, the following bodily changes occur:
- Growth of muscles and hair
- Growth of the penis and testicles
- Deepening of the voice
- Creation of sperm
- Enhancement of sex drive
While testosterone is primarily related to men, women produce the same hormone as well, although in smaller amounts. Similarly, it helps in body functioning as well as the maintenance of some female reproductive organs.
Because of its involvement with many bodily processes, alterations in the levels of testosterone can wreak havoc to one’s health.
Physiologically speaking, testosterone levels to decline with age. However, an abnormal decline in men’s testosterone levels can lead to infertility, diminished sex drive, bone loss, and low energy.
It can also lead to andropause or late-onset hypogonadism, which is characterized by the following signs and symptoms, apart from the ones stated above:
- Anemia
- Depression
- Poor concentration
- Loss of muscle mass
- Inability to have an orgasm
HIV/AIDS is another condition where testosterone levels are decreased.
In women, increase in testosterone levels can result to the development of Polycystic Ovarian Syndrome. This disorder is hallmarked by obesity, acne, blood sugar aberrations, facial hair growth, lack of menstruation, and infertility.
Hypothyroidism
What is Hypothyroidism?
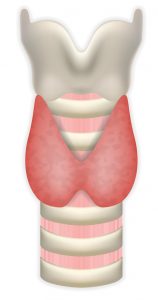
Hypothyroidism is a condition that develops when the thyroid gland, a butterfly-shaped organ located by the neck, is unable to produce the quantity of thyroid hormone that the body needs. This results in the slowing down of the body’s many processes, as thyroid hormone plays a major role in controlling energy use and organ functioning, among many other activities.
Hypothyroidism is more prevalent in women, and in individuals aged 60 and above. Other risk factors that lead to the eventual development of the disease include:
- Goiter or other thyroid-related problems
- Surgical removal of the thyroid gland
- Radiation treatment for the face or neck
- Family history of thyroid problems
- Pregnancy within the last 6 months
- Illnesses such as Turner’s Syndrome, Sjogren’s syndrome, Diabetes Mellitus, Lupus, Rheumatoid Arthritis, or Pernicious Anemia
Symptoms of hypothyroidism include the following:
- Goiter
- Cold intolerance
- Slow heart rate
- Weight gain
- Puffiness of the face
- Muscle and joint pain
- Constipation
- Dry hair and skin
- Decreased sweating
- Depression
Hypothyroidism and its Effects on Testosterone
Low levels of testosterone seen in hypothyroidism can be attributed to the poor responsiveness of Luteinizing hormone (LH) to the administration of Gonadotropin-releasing hormone (GnRH.)
According to a study by Tsutsumi and Webster, GnRH is the primary hormone that affects reproductive functioning. It works by stimulating the “anterior pituitary gland, which then creates and secretes LH and Follicle-stimulating hormone (FSH.)”
LH stimulates the release of sex steroids. In males, LH brings about the synthesis and secretion of testosterone. In females, the ovaries secrete testosterone, which is then converted into estrogen.
In hypothyroidism, LH responds poorly to the stimulation of GnRh. Expectedly, this occurrence leads to a decrease in free testosterone levels, which is defined as the amount of circulating or ‘unattached’ testosterone hormones in your body.
Note that the normal levels usually range from 300 to 900 nanograms per deciliter.
Because of the effects of hypothyroidism on the endocrine system as stated above, levels of free testosterone in the body are reduced. As indicated above, low levels of testosterone can lead to infertility, diminished sex drive, bone loss, and low energy.
But this is not all there is to it – low levels of testosterone can also lead to other health problems.
For one, low testosterone levels can lead to brittle bones, and such can lead to the development of osteoporosis later on in life.
Testosterone can also affect blood sugar levels, and this can lead to the development of diabetes mellitus in old age.
Cardiovascular health is also affected by testosterone, as a decrease in the levels of the said hormone has been associated with some higher adverse cardiovascular events.
This is often treated by correcting thyroid disorders through supplements or drug, or getting testosterone replacement therapy..
Hypogonadotropic Hypogonadism
Because hypothyroidism brings about fluctuations in hormonal levels, it also leads to the development of Hypogonadotropic Hypogonadism, a condition in men (and also women) where there is little or no production of sex hormones, it is also known as secondary hypogonadism or Gonadotropin deficiency.
This condition usually occurs because of problems in the pituitary gland or the hypothalamus, where there is lack of the following hormones that usually stimulate the testes or ovary. These vital hormones are GnRH, LH, and FSH.
However, in some male children with hypothyroidism, there is an elevation in follicle-stimulating hormone which is linked to an enlargement of the testes sans virilization.
Normally, the brain’s hypothalamus secretes GnRH, and this then stimulates the release of LH and FSH from the pituitary gland. These direct the testes in males and ovaries in females to proceed to the sexual development seen in puberty.
Alterations in this process, as seen in Hypogonadotropic hypogonadism, results in the lack of sex hormones.
This then thwarts normal sexual development and maturity.
Symptoms of hypogonadotropic hypogonadism in adults include mood changes, weight gain, decreased interest or energy, muscle mass loss, loss of libido/sexual drive, and lack of menstruation in women. If left untreated, these symptoms can lead to infertility, risk for fractures, and early menopause in women.
Hyperthyroidism
What is Hyperthyroidism?
Hyperthyroidism is a disorder wherein there is excess production of thyroid hormones. As a result, metabolism is increased. Commonly occurring in men and after age 60, symptoms of the disease include:
- Goiter
- Fast heart rate
- Palpitations
- Tremors, shaky feeling
- Heat intolerance
- Anxiety or irritability
- Concentration difficulties
- Increased appetite coupled with weight loss
- Insomnia
- Bulging eyes, in Graves’ disease
Hyperthyroidism and its Effects on Testosterone
As hyperthyroidism disrupts hormonal balance in the body, the condition results in the elevation of testosterone levels in the body. One of the reasons behind this is the enhanced responsiveness of Luteinizing hormone (LH) to Gonadotropin-releasing hormone administration.
Since LH stimulates the release of sex steroids, an increase in LH release consequently leads to an increase in testosterone levels in the body.
While normal levels of testosterone result in better bone density and strength, improved libido and sexual function, enhanced muscle strength, and protection from cardiovascular diseases, increased levels of testosterone can bring about the following adverse effects:
- Decrease in spermatogenesis or slowed development of semen inside the testes.
- Increased sebum production which can lead to the development of acne.
- Water retention and subsequent edema.
- Gynecomastia, or breast tissue enlargement, which can be accompanied by breast pain.
- Enlargement of the heart or hypertrophy, as seen in the study of Pirompol et al.
- Aggressive behavior; as testosterone has been known to affect the hypothalamus, amygdala, and periaqueductal gray, all of which are involved in the manifestation of human aggression.
- Increased rates of suicide in adolescents and young adults due to testosterone-related elevated aggression.
Hyperthyroidism also brings about an increase in the concentrations of Sex-Hormone Binding Globulin or SHBG. This protein binds to testosterone and other hormones, and transports these biologically-inactive hormones via the bloodstream.
An increase in SHBG means there is more testosterone in the body, which is of course a hallmark hormone elevation seen in hyperthyroid patients.
Other associated hormonal changes that occur with hyperthyroidism include:
Elevated Estradiol levels
Estradiol, also known as E2, is an estrogen primarily synthesized in the ovaries. This hormone is particularly increased during the reproductive years, with normal levels ranging from 0 to 30 pg/ml. Such concentrations are essential for the development of the vagina, fallopian tubes, uterus, and breasts.
While it is more common in women, minute amounts of estrogen are secreted by the testes as well. Normal levels for men range from 10 to 50 pg/ml.
Apart from affecting sexual development, Estrogens such as Estradiol are known to affect thyroid function as well. It increases the amount of thyroid-binding globulin, which necessitates the need for more thyroid hormone when it comes to treating hypothyroid women (compared to men.)
In a study by Abdel-Dayem and Elgendy, it was determined that estradiol treatment can bring out hyperactivity of the thyroid. Subsequently, a recent study by Santin and Furlanetto showed that estradiol, together with Estrogen, play a role in the development of goiter and thyroid carcinoma. Such can be attributed to the hormones’ ability to mediate cell cycle progression in thyroid cells.
Low responsiveness to Human Chorionic Gonadotropin (HCG) administration
HCG is an essential hormone for fertility. In women, it helps in the development of the egg in the ovary. It also prods the release of the developed egg during ovulation. In pregnant women, HCG is produced by the placenta. Medically, this hormone is used to induce ovulation and treat infertility in females.
In men, HCG plays a role in penile growth and testicular steroidogenesis. Medically, it is used to increase sperm count in adult males. For boys, HCG is used to help treat those with undescended testes.
As with most hormones, HCG is known to exert a thyrotrophic effect, meaning it can influence the secretory activity of the thyroid gland. In fact, its structure is similar to thyroid-stimulating hormone, and this could explain the HCG changes that occur with hyperthyroidism.
Radioactive Iodine Therapy and its Effects on Men
Radioactive iodine therapy is implemented in the diagnosis and treatment of patients with hyperthyroidism or thyroid cancer. As for diagnosis, it is used to determine thyroid function, as well as the size and location of the thyroid gland. As for treatment, I-131 is administered to destroy oversized and overactive thyroid tissue (as seen in hyperthyroidism,) or destroy cancer cells (as seen in thyroid cancer.)
Although RAI is successful in treating afflicted patients, it comes with a price. As with other therapies, RAI can bring about endocrine changes. Normally, elevations in follicle-stimulating hormone and Luteinizing hormone are observed. Reduction in inhibin B levels have been seen as well.
Impairment of spermatogenesis has also occurred in some men, with severity according to dose, up to two years after the end of RAI therapy. Impairment in the germinal and Leydig cell function also occurs, with recovery occurring after one and a half years of treatment.
According to the study done by Meikle, it has been noted that in more severe cases, high-level RAI therapy has been known to eventually lead to testicular germ cell damage.
Granted the close relationship of thyroid hormones and testosterone (among many other sex hormones,) RAI treatment is employed carefully in order to maintain the normal levels of other hormones in the body.
References:
Abdel-Dayem, M. M., & Elgendy, M. S. (2009). Effects of chronic estradiol treatment on the thyroid gland structure and function of ovariectomized rats. BMC Research Notes, 2, 173. http://doi.org/10.1186/1756-0500-2-173
Estradiol (Blood). (n.d.). Retrieved January 03, 2018, from https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=estradiol
Free Testosterone. (n.d.). Retrieved December 02, 2017, from https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=testosterone_free
Gonadotropins: Luteinizing and Follicle Stimulating Hormones. (n.d.). Retrieved January 03, 2018, from http://www.vivo.colostate.edu/hbooks/pathphys/endocrine/hypopit/lhfsh.html
Hypogonadotropic hypogonadism. (n.d.). Retrieved December 29, 2017, from http://www.umm.edu/health/medical/ency/articles/hypogonadotropic-hypogonadism
Hypothyroidism (Underactive Thyroid). (2016, August 01). Retrieved December 26, 2017, from https://www.niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism
Meikle, A. W. (2004). The interrelationships between thyroid dysfunction and hypogonadism in men and boys. [Abstract]. Thyroid, 14, 17-25. Retrieved December 3, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/15142373
Osterberg, E. C., Bernie, A. M., & Ramasamy, R. (2014). Risks of testosterone replacement therapy in men. Indian Journal of Urology : IJU : Journal of the Urological Society of India, 30(1), 2–7. http://doi.org/10.4103/0970-1591.124197
Pirompol, P., Teekabut, V., Weerachatyanukul, W., Bupha-Intr, T., & Wattanapermpool, J. (2016). Supra-physiological dose of testosterone induces pathological cardiac hypertrophy [Abstract]. Journal of Endocrinology, 229(1), 13-23. Retrieved January 4, 2018, from http://joe.endocrinology-journals.org/content/229/1/13.long#ref-list-1
Santin, A. P., & Furlanetto, T. W. (2011). Role of Estrogen in Thyroid Function and Growth Regulation. Journal of Thyroid Research, 2011, 875125. http://doi.org/10.4061/2011/875125
Tsutsumi, R., & Webster, N. J. G. (2009). GnRH Pulsatility, the Pituitary Response and Reproductive Dysfunction. Endocrine Journal, 56(6), 729–737.
Voigt, W., Maher, G., Wolf, H. H., & Schmoll, H. J. (2007). Human chorionic gonadotropin-induced hyperthyroidism in germ cell cancer–a case presentation and review of the literature. Onkologie, 30(6), 330-334. Retrieved January 4, 2018, from https://www.ncbi.nlm.nih.gov/pubmed/17585415.
No Comments